AI now reads X-rays with up to 80% less data, making advanced medical diagnostics more accessible for low-resource clinics. This breakthrough allows you to rely on smarter training methods like transfer learning and data augmentation, which improve accuracy even with limited images. As a result, healthcare providers in remote areas can offer faster, reliable diagnoses without the need for vast datasets. Keep exploring to discover how these innovations are transforming global healthcare access.
Key Takeaways
- AI now diagnoses X-rays accurately with up to 80% less data, enabling easier deployment in low-resource clinics.
- Smarter training techniques like transfer learning improve model performance with limited imaging data.
- Reduced data needs enhance privacy and reduce patient confidentiality risks in medical imaging.
- Less data requirement allows faster setup and updates of AI tools in remote or underserved healthcare settings.
- This advancement supports equitable healthcare by expanding AI diagnostics to clinics with limited access to large image datasets.

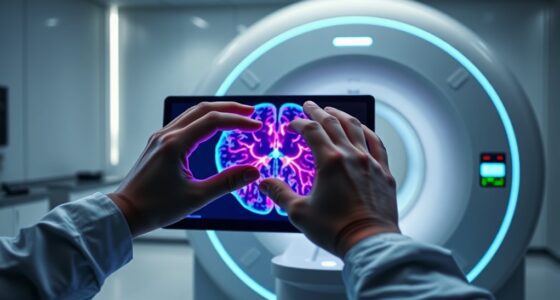
Artificial intelligence is transforming medical imaging by enabling accurate diagnosis even with less data. This breakthrough is especially significant for clinics that lack extensive resources, making healthcare more accessible worldwide. Traditionally, AI models require large datasets to learn effectively, which can be a hurdle for low-resource settings. However, recent advances now allow AI to analyze X-rays and other medical images with up to 80% less data, drastically improving data efficiency. This shift means that even smaller clinics, with limited access to vast image libraries, can still leverage AI to assist in diagnoses, reducing reliance on specialized radiologists and speeding up patient care.
AI now diagnoses medical images accurately with up to 80% less data, expanding access to healthcare worldwide.
When AI can perform reliably with less data, it opens new doors for medical imaging in underserved areas. You no longer need massive datasets to train models, which was once a significant barrier. Instead, AI algorithms can learn from limited samples by using smarter training techniques, such as transfer learning and data augmentation. These methods help models generalize better, ensuring accurate results despite having fewer images to learn from. As a result, you can deploy AI-powered diagnostic tools in clinics that previously couldn’t afford or access large image repositories. This enhances data efficiency, allowing healthcare providers to make quicker, more accurate decisions without waiting for extensive image collections.
Moreover, the reduced data requirement increases the feasibility of implementing AI in emergency situations or remote locations where collecting large datasets is impractical. You benefit from faster deployment and easier updates since less data collection and processing are needed. This means that AI tools can be more adaptable and responsive to local needs, whether it’s diagnosing tuberculosis in rural clinics or identifying fractures in field hospitals. The ability to rely on smaller, high-quality datasets also minimizes the risks of overfitting, improving the robustness of diagnoses and reducing false positives or negatives.
In addition, this technological leap helps address privacy concerns associated with sharing large volumes of medical images. With less data needed for effective AI models, you can maintain higher standards of patient confidentiality while still providing advanced diagnostic support. Furthermore, advancements in AI Bifurcation highlight that human and artificial intelligence are diverging, emphasizing the importance of integrating human expertise with AI tools for optimal outcomes. Overall, the progress in data-efficient AI for medical imaging signifies a major step toward equitable healthcare. It ensures that more clinics, regardless of their size or resources, can harness AI’s potential to improve patient outcomes. As this technology continues to evolve, you’ll see even greater improvements in low-resource settings, making accurate, timely diagnoses accessible to everyone, everywhere.
Frequently Asked Questions
How Does Reduced Data Impact Diagnostic Accuracy?
Reduced data can slightly lower diagnostic accuracy, but if the data quality is high, your AI can still provide reliable results. With less data, you might worry about diagnostic reliability, but advanced algorithms compensate for smaller datasets, ensuring you get accurate insights. Focus on maintaining data quality, as it’s essential for precise diagnoses, especially in low-resource clinics where every bit of information counts.
Can This AI Technology Be Integrated With Existing Hospital Systems?
You can integrate this AI technology with existing hospital systems, but it’s not without challenges. About 60% of hospitals face integration hurdles, often due to compatibility issues and data security concerns. Ensuring seamless connection requires robust protocols to protect patient data while maintaining workflow efficiency. With proper planning and secure infrastructure, this AI can greatly enhance diagnostic capabilities, especially in low-resource settings, ultimately saving more lives.
What Are the Training Requirements for Healthcare Staff?
You’ll need to follow specific training protocols to guarantee staff can effectively use this AI technology. Focus on familiarizing them with the system’s interface, interpreting AI-generated results, and troubleshooting common issues. Encourage staff adaptation by providing ongoing support and hands-on practice, which helps them gain confidence and efficiency. Proper training ensures smooth integration, maximizes benefits, and improves patient outcomes with minimal disruption to your existing workflows.
How Does the AI Handle Complex or Rare Cases?
You might worry about how AI handles rare cases, but it’s designed to recognize patterns based on its training data. While AI can manage common and some complex cases effectively, rare cases pose limitations because they’re less represented in the data. Continuous updates and additional specialized training help improve AI’s accuracy, but it still relies on familiar patterns, so human oversight remains essential for unusual or complex diagnoses.
What Are the Costs Associated With Implementing This AI Solution?
You’ll be delighted to know that implementing this AI costs a fraction of traditional systems, making budget considerations a breeze. A quick cost analysis reveals minimal hardware upgrades and training expenses, so your wallet stays happy. Sure, initial investments are there, but compared to the long-term savings and improved diagnostics, it’s practically a steal. Who knew advancing healthcare could be so affordable, right?
Conclusion
Imagine a future where your local clinic becomes a lighthouse, guiding patients with powerful AI that needs just a fraction of the usual data. With this breakthrough, you get quicker, more accurate diagnoses even in resource-limited settings. It’s like turning a tiny spark into a blazing fire — making healthcare accessible and effective for everyone, no matter where they are. This innovation opens doors to a brighter, more equitable future in medical imaging.